Can Whistleblowing Enhance Patient Safety?

Earlier this month, U.K. Health Secretary Jeremy Hunt proposed the creation of an Independent “Healthcare Safety Investigation Branch” to offer legal protection to so-called whistleblowers who draw attention to mismanagement by medical practitioners that compromises patient safety. The committee will operate from April 2016 and will at first focus on human error in maternity units, he said.
Additionally, hospital deaths will be reviewed independently from April 2018, Hunt has proposed, saying: “It is a scandal that every week there are potentially 150 avoidable deaths in our hospitals and it is up to us all to make the need for whistleblowing and secrecy a thing of the past as we reform the NHS and its values and move from blaming to learning.”
The measures are hardly surprising when considering the global push to improve patient safety records. In March, the “Patient Safety 2030” report was presented at a global conference in London, stating that 5 percent of the total number of patient safety incidents are actually reported to authorities due to a culture of staff “fearfulness.”
It’s additionally been suggested across various medical circles in the Western world that the industry must immediately put an end to the “cover-up culture” to help prevent unnecessary and avoidable harm to patients.
This begs the question: Is the focus on punitive measures diverting from the underlying causes of the problem?
“It is imperative to investigate clinical incidents rigorously to identify root causes and to learn from these, but at present there appears to be a disproportionate focus on punitive measures,” Dr. Richenda Tisdale of the Medical Protection Society said in a piece written for GPOnline.com on March 21, arguing that a cultural shift can’t be spurred by changes in legislation, alone.
According to Tisdale, doctors already have a duty to “promote and encourage a culture that allows all staff to raise concerns openly and safely,” under “Good Medical Practice” rules enforced by the General Medical Council.
While additional legislation may help improve patient safety, the cultural shift will require a far more rigorous plan involving various medical actors and a system-approach across the board, Tisdale said, adding, “a doctor involved in a clinical incident can face a complaint, disciplinary, regulatory and criminal investigation simultaneously, even though the issue may be a system failure of which they are one small part.”
Additionally, once information is shared and action is taken against a particular doctor or institution, networks that are already in place should be utilized to share learning points at both the local and national levels to ensure the dissemination of information more widely. This approach is less focused on the “punishment” aspect of identifying malpractice, placing more emphasis on how to learn from mistakes.
Indeed, a multi-faceted approach to patient safety is at the very core of the global movement to foster it. In a piece published in The Guardian, former U.K. health minister Lord Darzi proposed four “novel projects” that go above and beyond punitive punishment.
While acknowledging that medical staff are oftentimes put off from reporting human error for fear of recrimination, in this particular piece, Darzi argues that novel systems could in fact yield immediate, positive effects on the field.
They include: a Heads-Up mechanism, which aims to present a list of reported problems from the previous day to medical practitioners on one sheet of A4 — anything from a broken piece of equipment to a patient “almost being given the wrong drug”; Hark, a clinical task management tool; a Hospital Drugs Chart put together by designers, behavioural scientists and academics; and Ambulance Redesign.
“While a culture of openness and reflection is clearly a good thing, the practicalities are somewhat more complex,” Dr. Tinsadale said on GPOnline, reflecting the need to focus on several mechanisms to combat patient safety, rather than just one, in isolation.
“Support and training for those conducting investigations, a moratorium in the regulation faced by the profession and stricter guidance for the Crown Prosecution Service meaning that fewer doctors face unnecessary criminal action may be more effective.”
المزيد أخبار

يشارك ويش في حوارات خبراء حول الصحة والسياسات والرفاه في شهر ديسمبر
اقرأ أكثر...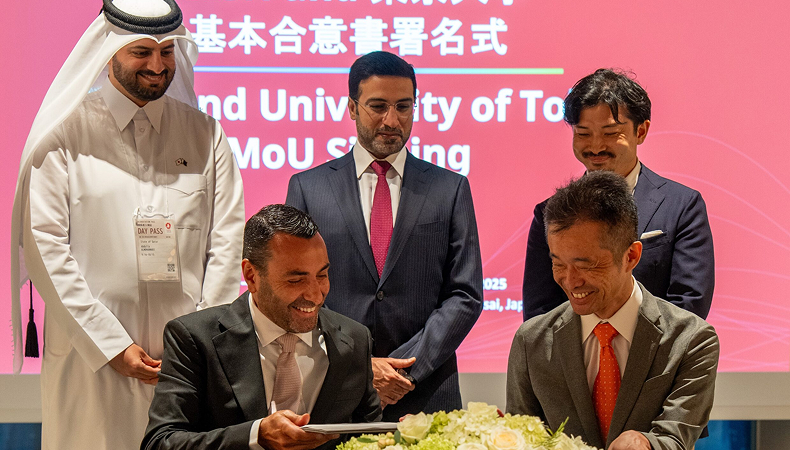
مؤتمر “ويش” وجامعة طوكيو يوقعان مذكرة تفاهم محورية لتعزيز السياسات الصحية العالمية خلال معرض أوساكا إكسبو
اقرأ أكثر...
ويش يقود جهود التحرك لمكافحة أمراض القلب والأوعية الدموية خلال القمة العالمية للقلب 2025
اقرأ أكثر...